By NEELU PRASAD
Assistant Professor
Department of CVT
School of Health Sciences
Sushant University
Introduction
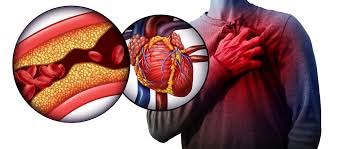
Heart disease remains one of the leading causes of mortality worldwide. While many are familiar with the classic signs of a heart attack—crushing chest pain, shortness of breath, and profuse sweating—there is a lesser-known but equally dangerous form: the silent heart attack. Unlike typical heart attacks, silent heart attacks (also known as silent myocardial infarctions or SMIs) occur with minimal or no recognizable symptoms. As a result, they often go unnoticed and untreated, leaving individuals vulnerable to serious complications.
This article aims to explore the phenomenon of silent heart attacks in detail, including their causes, symptoms, risk factors, diagnostic challenges, prevalence, and strategies for prevention and management.
What is a Silent Heart Attack?
A silent heart attack is a type of myocardial infarction that occurs without the typical, dramatic symptoms associated with heart attacks. These events may be painless or accompanied by vague symptoms that are easily dismissed or misattributed to less serious conditions such as indigestion, fatigue, or anxiety.
Key Features:
- Lack of chest pain: Unlike traditional heart attacks, chest pain may be mild or entirely absent.
- Unrecognized symptoms: Symptoms such as shortness of breath discomfort in the arms or jaw, and light-headedness may be subtle.
- Delayed or missed diagnosis: Many cases are discovered only during routine tests like an ECG or echocardiogram.
Causes and Pathophysiology
Silent heart attacks, like traditional ones, are caused by the obstruction of blood flow to a part of the heart muscle, usually due to a blockage in one or more coronary arteries. This blockage can result from:
- Atherosclerosis: Build-up of plaque in the arteries, leading to reduced blood flow.
- Coronary artery spasm: Sudden narrowing of a coronary artery.
- Blood clot formation: Thrombosis that blocks blood flow.
The reason silent heart attacks are not felt as acutely may be due to differences in nerve function or altered pain perception. People with conditions such as diabetes are particularly susceptible because of diabetic neuropathy, which impairs their ability to feel pain.
Symptoms: What Makes Them “Silent”
Though termed “silent,” these heart attacks are not entirely symptom-free. The issue is that symptoms are often so mild or atypical that they go unnoticed or are misinterpreted. Common signs include:
- Mild or fleeting chest discomfort
- Fatigue or general weakness
- Shortness of breath
- Nausea or indigestion-like sensation
- Pain or discomfort in the jaw, neck, or arms
- Cold sweats
- Light-headedness or dizziness
Risk Factors
Several risk factors increase the likelihood of silent heart attacks, many of which overlap with those of traditional heart attacks:
- Diabetes: Neuropathy can dull pain sensation, masking symptoms.
- Hypertension: High blood pressure damages arteries and increases cardiac workload.
- High cholesterol: Contributes to atherosclerosis.
- Smoking: Damages the cardiovascular system.
- Obesity and sedentary lifestyle
- Age: Risk increases with age.
- Gender: Women may experience more atypical symptoms.
- Family history of heart disease
Diagnosis: The Role of Investigations
Because silent heart attacks often go unnoticed, diagnostic tools play a crucial role in identifying them:
1. Electrocardiogram (ECG)
Can reveal abnormalities such as Q waves or ST changes indicative of past myocardial damage.
2. Echocardiogram
Assesses heart wall motion abnormalities, which may suggest prior damage.
3. Blood Tests (Troponin levels)
Useful for detecting heart muscle damage, especially in acute phases.
4. Stress Testing and Cardiac MRI
Helpful for identifying areas of ischemia or infarction.
Prevalence and Impact
Silent heart attacks are more common than many people realize. According to the American Heart Association:
- Nearly 1 in 5 heart attacks is silent.
- People with silent heart attacks have a higher risk of sudden cardiac death.
- These heart attacks are often only discovered later, during imaging or routine cardiac assessments.
A 2022 study by the Journal of the American College of Cardiology found that among diabetics, over 50% of heart attacks were silent. In India, with a high prevalence of diabetes and hypertension, this figure could be even more significant. An AIIMS study in 2021 reported a 25% prevalence of undiagnosed myocardial infarctions in individuals over 45.
Complications and Long-Term Effects
Despite their subtle onset, silent heart attacks can have serious consequences:
- Left ventricular dysfunction
- Heart failure
- Arrhythmias (e.g., atrial fibrillation)
- Increased risk of subsequent heart attacks
- Sudden cardiac death
Undiagnosed damage from a silent heart attack may compromise heart function and reduce life expectancy.
Prevention and Lifestyle Modifications
Preventing silent heart attacks involves managing risk factors and making lifestyle changes:<//p>
1. Regular Screenings
Routine ECGs, cholesterol checks, and blood pressure monitoring are vital for at-risk individuals.
2. Healthy Diet
A heart-friendly diet includes:
- Low saturated fats
- High fiber
- Plenty of fruits, vegetables, and whole grains
- Limited sodium intake
3. Exercise
At least 30 minutes of moderate exercise (e.g., brisk walking) five days a week is recommended.<//p>
4. Avoid Tobacco and Limit Alcohol
Smoking cessation and moderation in alcohol intake are essential.
5. Stress Management
Techniques like yoga, meditation, and therapy can help control blood pressure and emotional well-being.
6. Medication Adherence
Ensuring compliance with medications for diabetes, hypertension, and cholesterol is crucial.
Importance of Public Awareness
Public health initiatives should aim to:
- Educate about the signs of silent heart attacks
- Encourage regular health check-ups, especially for high-risk groups
- Promote heart health from an early age
Campaigns tailored to rural and urban populations in countries like India can help bridge the gap in cardiac care access and awareness.
Conclusion
Silent heart attacks pose a hidden but significant threat to public health. Because they lack obvious symptoms, they are often overlooked, resulting in delayed treatment and worse outcomes. Increased awareness, preventive strategies, and early diagnosis through regular screenings can save lives. Individuals must be proactive in their healthcare, particularly those with known risk factors. In the battle against cardiovascular disease, listening to what your body doesn’t say may be just as important as recognizing what it does.
References
- American Heart Association. (2022). Heart Disease and Stroke Statistics.
- AIIMS. (2021). Study on Undiagnosed Myocardial Infarctions in Indian Adults.
- Journal of the American College of Cardiology. (2022). Silent Myocardial Infarctions in Diabetic Patients.
- World Health Organization. (2021). Global Report on Cardiac Diseases.
- National Institute of Health. (2020). Cardiovascular Health Data Trends.
